Introduction of department
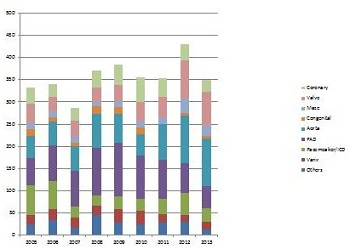
Cardiovascular surgery is one of our main department. Our cardiovascular surgery covers all fields of cardiovascular diseases, including coronary artery disease, valvular heart disease, aortic disease, arrhythmia and peripheral artery disease. Among them, our speciality is valvular heart disease, such as mitral valve plasty and bioprosthetic replacement for aortic valve stenosis. Transcatheter aortic valve implantation (TAVI) is also planned to perform instead of surgical aortic valve replacement. Maze surgery is our main favorite for chronic atrial fibrillation. Our procedure is well known as the Hiroshima procedure. Aortic surgery became common surgery after induction of thoracic endovascular aneurysm repair (TEVAR). The number of TEVAR exceeds 50 cases per year. We can performed hybrid surgery for complicated type A aortic dissection or huge aortic arch aneurysm using open replacement and TEVAR. We also performed peripheral arterial disease using hybrid procedure such as stent dilatation for iliac artery and distal bypass using in-situ saphenous in our hybrid operation room.
Research content
What's an aneurysm? Q and A
We started endovascular aneurysm repair of abdominal and thoracic aorta.
This article explains what aortic aneurysm is.
Introduction
The aorta is the main artery in the body. It runs from the heart, through the chest and abdomen and supplies branches to all the major organs. An aortic aneurysm is a general term for an enlargement (dilation) of the aorta to greater than 1.5 times normal size (normal size of a thoracic aorta and an abdominal aorta are 3cm and 2cm respectively).
This is a result of weakening of the artery wall, which then stretches due to the pressure of the blood flowing through the aorta, to form an aneurysm. The larger the aneurysm is, the greater the chance that it might rupture (burst) and if an aneurysm ruptures it can be fatal.
Medical therapy of aortic aneurysm involved strict blood pressure control. This does not treat the aortic aneurysm per se, but control hypertension within tight blood pressure parameters may decrease the rate of expansion of the aneurism. Once an aorta enlarges, no medical therapy can reduce its size. Only surgical therapy can prevent further enlargement of aorta.
Decisions on if and when to repair an aortic aneurysm are based on the balance between the risk of aneurysm rupture without treatment versus the risks of the treatment itself. There are two approaches for surgical repair; Open surgery and endovascular repair.
Diagnosis
The abdominal (thoracic) aorta reaches 3cm (4cm) in diameter, it is classified as an aneurysm.
Indication
Surgical repair should proceed when the abdominal (thoracic) aorta reaches a diameter 4cm (5cm). It is also indication of surgical repair that the rate of enlargement of aorta is more than 0.5mm per half year.
Treatment
- Medical therapy
Strict blood pressure control
Normalizing your lifestyle habit (smoking, exercise etc)
Reducing stressor
Please follow instruction of your home physician or cardiologist. - Aortic replacement (open surgery)
Surgery for aortic aneurysms involves opening the chest or the abdomen and replacing the aorta and inserting a synthetic aorta. The procedure has risks, generally, mortality for abdominal aneurysm is approximate 1%, for thoracic aneurysm is 5-10%.
When rupture occurs, massive internal hemorrhage results, can be fetal. Even if emergency surgery can undergo, the mortality is very high. - Endovascular aneurysm repair
A small surgical incision near the groin is put, to find femoral artery, and a surgeon insert a stent and a synthetic graft through the cut into the artery. Then open the stent to cover your aneurysm. Eventually, the endograft, once in place, acts as an artificial lumen for blood to flow through, and not into the surrounding aneurysm sac.
Some situations are contra-indications.
• There are important branches near aneurysm.
• A tortuous aorta.
However, newly developed techniques could be solution of above cases. One is a specially designed graft, another is hybrid procedure (the prior placement of surgical bypass graft to important branch allows to deployment of the endograft at the level that would otherwise not be possible).
Because endovascular aneurysm repair have a short history, the long term result is unknown. Especially an endoleak, which is a leak into the aneurysm sac after endovascular repair, is one of big problems of the procedure.
For the above reasons, we should discuss before select the procure to repair the aneurysm.
Q and A
Q1. Medication can reduce aneurysm size?
A1. Unfortunately, there is no medicine that can reduce aneurysm size at the moment. Strict blood pressure control might prevent enlarge aneurysm size more. Only surgical repair can remove the risk of aneurysm rupture.
Q2. I have an aneurysm. How much blood pressure should I control?
A2. You must control your blood pressure strictly. Please keep systolic (higher) blood pressure less than 130mmHg.
Q3. I have an aneurysm. Can I exercise?
A3. If your home physician told you that your aneurysm size didn’t reach the size it is recommended repair, you can do light exercise except for extreme one. However the doctor recommend surgical repair, you can just walk slowly.
During exercise, if you feel pain or high blood pressure, please stop exercise and consult your physician.
Q4. My home doctor told me `If you don’t undergo surgery to repair aneurysm, the risk of aneurysm rupture is very high.’ But I don’t feel any symptom at all. Is that true?
A4. The final decision is yours. Please understand both risks of rupture and surgery. And then please talk to your doctor again and decide.
Q5. My home doctor told me I have thoracic aortic aneurysm near neck vessels and the risk is too high to do operation due to comorbidity. How about endovascular repair?
A5. We need check your aneurysm on CT angiography before give our advice. If CT angiography indicates the risk of rupture is high, we consider surgical repair. We will decide whether open surgery or endovascular repair is suitable for you after we evaluate your aneurysm type, size and place and your condition.
Abdominal Aortic Aneurysm Repair –EVAR(Endovascular aneurysm repair)-
What is an abdominal aneurysm?
The abdominal aorta is the main bloody vessel in the abdominal cavity that transmits oxygenated blood from the thoracic cavity to the organs within the abdomen and to the lower limbs.
An abdominal aortic aneurysm (AAA) is dilation or bulging of that aorta. The most common cause of aortic aneurysms is ``hardening of the arteries`` called arteriosclerosis.
Most AAAs produce no symptoms (asymptomatic) and are discovered incidentally when an imaging test of the abdomen (CT scan or ultrasound) is performed at medical check or other purpose. However, as AAAs expand, they may become painful lead to pulsating sensations in the abdomen. The risk of rupture is high in a symptomatic aneurysm.
If the diagnosis is missed or if the patient does not present for care, the aneurysm can burst or rupture causing potential catastrophe and death. The most important thing is to treat aneurysms before rupture. AAA that size is more than 4-4.5cm is recommended to repair to prevent rupture.
Treatment
There are two approaches for repair. The first is the traditional surgical approach. A large incision is made in the abdomen, the AAA is identified and cut out or resected. The missing piece replace with a synthetic graft.
The second approach is placing an endovascular graft. A catheter or tube is threaded into the femoral artery in the groin and the graft is positioned so that it spans and sits inside the aneurysm and protects it from expanding. That approach is called as EVAR (endovascular aneurysm repair).
The approach to treatment needs to be tailored to the individual patient and very much depends on the location, size, and shape of the aneurysm.
Please don`t hesitate to contact to us if any query about AAA and endvascular graft.
Minimary Invasive Cardiac Surgery (MICS) ―By MICS, social rehabilitation will also be promptly―
In cardiac surgery, a median sternotomy incision that vertically the entire sternum is standard. When all the sternum incision, about 3 months, you could not have a heavy object of 10Kg or more and hard exercise would be difficult. Three months later, limitation of motion is released basically. Young people will take the time to social rehabilitation. Elderly people will take some time still to return to everyday life. In Hiroshima University Hospital, for cases that are suitable, we perform "MICS". However, in the complex case we have determined that the difficulty in MICS, we will make an incision in a conventional manner without unreasonable. We considered in conjunction with the patient. We will choose the method that benefit than suitable for disease states.
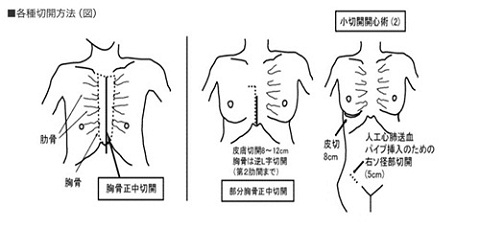
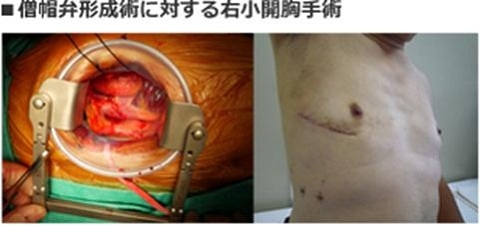
Specifically, in congenital heart disease and mitral valve disease surgery, we are doing a heart surgery under direct vision, either under the right breast done in small thoracotomy, or by the partial sternotomy with a small incision of the midline, under endoscopic assist.
In aortic valvular surgery, we have been partial sternotomy in small incision of the midline.
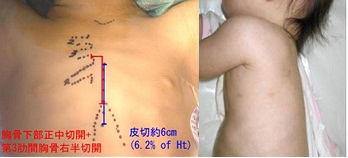
Minimally invasive congenital cardiac surgery
In our department, we have conducted a pediatric congenital heart disease surgery and adult congenital heart disease surgery.
In the pediatric cardiovascular surgery, in safety first, we are the surgery to minimize the burden on the children (MICS, Minimally Invasive Cardiovascular Surgery).
Specifically, if catheterization treatment is unsuitable for children, for atrial septal defect (ASD), we do the surgery in the middle of the chest skin incision only about 6% of the length of the height (If the child\'s height is 100cm, it is 6cm), without other sites incision (groin, neck etc.).Generally, using the clinical path, children are discharged from the hospital in four days.
Patent ductus arteriosus (PDA) is, if it is too thick catheter therapy is unsuitable, by only very small incision (about 1.5cm) of the left chest, a hole of 2 to 4 locations only, and a combination of thoracoscope, closed. Usually, children were discharged from the hospital in the next day because the chest did not cut large. Even if children are grown, they have no deformation of the thorax and wound do not stand out.
Adult congenital heart disease is a group of diseases that must be carried out treatment under close cooperation of adult cardiovascular surgeons and pediatric cardiovascular surgeons.
Always in our department, we are doing the medical care as a team. Even for atrial fibrillation and atrial flutter that are often complicated in adult congenital heart disease, aggressively incorporating the Maze procedure, we will have made a better treatment.
Surgical Treatment of Atrial Fibrillation
Usually, medications (drug therapy) are employed for the treatment of arrhythmia. But there are some drug refractory arrhythmias. In such case, we employed some invasive therapy as a second step.
For the treatment of ‘atrial fibrillation(AF)’, that is one of a kind of heart arrhythmia, there also be some invasive treatment. One arm is ‘catheter ablation’ and another is ‘surgical procedure’.
Based on the Japanese Guideline of JCS, the catheter ablation is one of the less invasive treatment and good for lone (without structural heart disease) AF and for ‘paroxysmal’ AF. But for valvular AF (with structural heart disease) and permanent/long-standing AF, the surgical procedure is suitable.
The surgical procedure of the treatment AF is called ‘maze’ procedure because of it’s incision line on the atrium. The original maze procedure was developed in USA by Prof. Cox at the end of 1980’s. In our hospital, we have developed a simplified, less invasive modified-maze procedure at 1990’s. We have performed this less invasive surgical procedure for long time with some improvement and nowadays AF diminishing rate have been achieved up to 90% with long-term outcomes. These results have been reported in several scientific journals.
http://arrhythm.umin.jp/treatment/surgery/simple.html
CIED lead extraction with excimer laser sheath
The troubled lead of CIED (Cardiac Implantable Electrical Device: ex. Pacemaker, Implantable Cardioverter Defibrillator, and Cardiac Resynchronizing Device) often should be removed completed for saving patients’ life. The most important cause of lead trouble is infection around these devices. If the infectious materials are leave, it can be fatal for those patients.
In our hospital, we can provide for the solution for troubled lead because our hospital acquires the institutional authorization to the lead extraction procedure with excimer laser sheath.
【Peeling-off the adhesion with laser】

Introducing the laser sheath
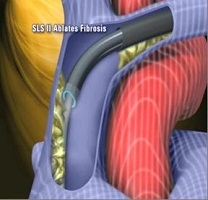
Irradiating the laser from the sheath
Coronary artery bypass grafting without extracorporeal circulation
Coronary artery bypass grafting (CABG) is one of the treatment for coronary artery disease. Coronary artery supply blood to heart and stenosis and/or occlusion of coronary arteries cause angina (chest pain) and myocardial infarction, and often result in death.
Indications of CABG are as follows:
- 3 vessel disease (all coronary arteries have stenosis more than 75% or occlusion)
- 2 vessel disease with left descending artery lesion (main coronary artery)
- Left main trunk disease
- Requiring any intervention, but Not applicable to percutaneous coronary intervention.
Etc.
Procedure of conventional CABG consists of :
- Harvesting graft (left/right internal thoracic artery, radial artery, gastroepiploic artery and saphenous vein)
- Establish extracorporeal circulation (ECC) (cardiopulmonary bypass, CPB)
- Arrest and protect heart and perform anasotmosis a graft with a native coronary artery
- Restart heart
- Removing ECC
In our institute off-pump coronary artery bypass grafting (OPCAB), which does not use ECC, has been introduced since 2005 and almost all elective cases undergo this procedure.
During OPCAB, heart is moving and we use several devices to accomplish the anastomosis, including stabilizer, shunt tube and CO2 blower.
In Japan, 60% of cases underwent OPCAB and achieved successful results. There are several advantages in OPCAB compared with conventional CABG. First, OPCAB does not require ECC which affects on the whole body and deteriorates any visceral function with cytokine storms, therefore, patients could recover earlier after OPCAB surgery. Second, despite there are controversial discussion, the incidence of stroke would be lower in OPCAB than conventional CABG.
Anastomosis in OPCAB is more difficult than that in conventional CABG, which requires skillful techniques, however, almost all cases accomplished OPCAB when we planned to perform it.
Graft selection is associated with patients’ prognosis and we usually use bilateral internal thoracic artery. However, we discuss which graft we use and where we anastomose in each patient and decide the best combination of bypass grafts.
A saphenous vein graft had inferior results to arterial grafts, but in some case we have to use it. At that time, we investigate the whole leg and choose the best saphenous vein.
The patency of coronary artery bypass grafting (CABG) is usually assessed by postoperative coronary angiography (CAG), which is reliable but not ideal because cardiac surgeons would prefer to know the condition of coronary artery perfusion during the operation. Surgeons commonly determine the success of a graft anastomosisby direct palpation. However, this technique is subjective, indirect and unreliable. Intraoperative manual diagnosis cannot accurately predict when revision of a graft is necessary to avoid graft occlusion. There are several techniques for graft assessment during the operation: thermal CAG using an infrared camera, laser-assisted indocyanine green angiography, electromagnetic flow meters, transittime flow meters (TTFMs), pulsed Doppler flow meters and colour pulsed Doppler. We have introduced a triangular-shaped silicone and gel interposed between an echo probe and a bypass graft as a means of recording graft flow. This technique guarantees the patency of bypass grafting and our overall patency after postoperative coronary angiography is approximately 98%, which is affected by our challenging spirits to anastomose of grafts to more difficult, small and poor coronary arteries.
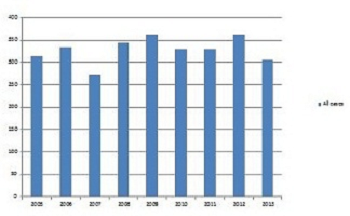
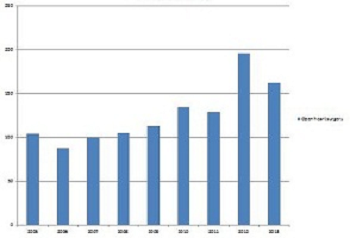
Treatment achievements
All cases
Open heart surgery

 Home
Home