Approximately 20 million people are diagnosed with cancer every year, and recent advances in cancer treatment have increased survival rates. However, most women undergoing treatment for cancer are at risk of fertility loss. While there are many options for fertility preservation (FP), the psychological distress associated with cancer diagnosis and treatment negatively affects the ability to make informed decisions about FP.
Hiroshima University researchers have developed, tested and validated a survey-based scale to systematically assess nursing practices that support FP decision-making in women with cancer, in Japan. This scale may be able to evaluate and enhance nursing practices that support FP measures.
Their work was described in a study published in the Asia-Pacific Journal of Oncology Nursing on December 2, 2025.
“Although fertility preservation is increasingly recognized as an important issue in cancer care, nursing support for FP decision-making has remained inconsistent and poorly standardized,” says Kazuaki Tanabe, professor at the Graduate School of Biomedical and Health Sciences, and corresponding author of the study. “This is important because nurses are often the first healthcare professionals to interact with patients, and insufficient or delayed support can result in women missing the opportunity to preserve their fertility during cancer treatment.”
Currently, standardized assessment tools for evaluating nursing support for FP are unavailable.
To develop the scale, the researchers conducted a literature review of papers in Japanese and English to clarify nursing practices that support FP decision-making, accounting for best practices, international perspectives, and the cultural context of Japan. The initial items on the scale were reviewed by a panel of experts who had more than 5 years of clinical or educational experience caring for women with cancer. The items were revised to improve clarity and ease of response.
From these evaluated items, a draft scale was prepared. The draft scale was in turn reviewed by another panel of six experts, two of whom evaluated the initial items. Once the scale was finalized, it was evaluated for reliability and validity. This took the form of a cross-sectional questionnaire across 450 institutions designated as part of Japan's national cancer control framework.
The cohort was divided into a group for exploratory factor analysis (EFA) — which identifies the underlying relationships between measured variables — and another group for confirmatory factor analysis (CFA) — which tests whether the data fit the relationships hypothesized from the EFA. The scale itself consisted of 22 items each scored between 1 to 5. Total scores ranged between 22 and 110, with higher scores indicating higher levels of FP-related nursing practice.
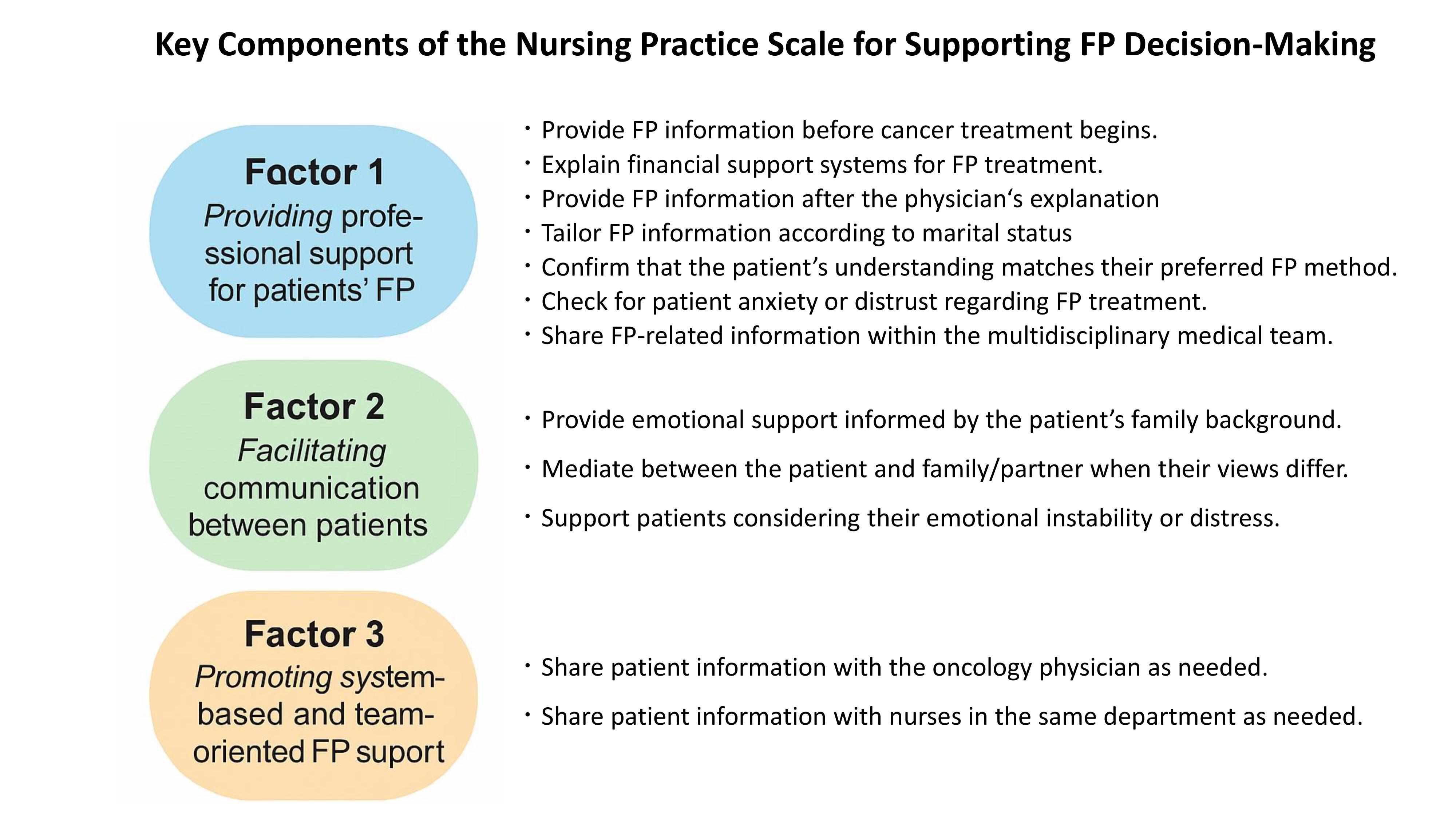
For the EFA group, 282 valid responses were received out of 817 distributed questionnaires; for CFA, 318 valid responses out of 744 questionnaires. “We developed a reliable and valid 12-item scale that captures three essential dimensions of nursing practice: professional decision-support, facilitation of communication between patients and families, and system- and team-based collaboration. By making these practices visible, the scale provides a concrete foundation for improving patient-centered, shared decision-making in oncology care,” Tanabe explains.
The three essential components of nursing practice supporting fertility preservation decision-making (Kazuaki Tanabe).
Tanabe continues, “A striking finding of this study is that nursing practices supporting fertility preservation decision-making can be clearly organized into three key factors: (1) professional support for fertility preservation decision-making, (2) support that understands and bridges the perspectives of patients and their families, and (3) the establishment of system-based and team-oriented approaches that make fertility preservation possible. Together, these three factors highlight that effective fertility preservation support requires not only individual nursing skills, but also communication and team-based systems working in harmony.”
“The next step is to apply this scale in clinical practice and nursing education to identify strengths and gaps in fertility preservation support,” Tanabe concludes. “Ultimately, the goal is to use this tool to improve the quality and consistency of nursing support, foster interprofessional collaboration, and ensure that women with cancer can make informed, value-based decisions about their reproductive future without regret.”
The research team includes Mikako Yoshihara, Chie Teramoto, Hiroyuki Sawatari, Ruxin Lei, and Hisae Nakatani at Hiroshima University.
This study was supported by The Yasuda Medical Foundation (2022Y-22).

 Home
Home