Tissue-Engineered Cultured Cartilage Transplantation: Putting Cultured Cartilage Where It Needs To Be Through Magnetic Force

In this edition of Research NOW, we interviewed Professor Mitsuo Ochi* of the Department of Orthopaedic Surgery in Programs for Applied Biomedicine at the Graduate School of Biomedical Sciences.
*Professor Ochi also serves as the Executive of Medical Affairs, and the Director of the University Hospital. We will, however, refer to him as "Professor" in this interview
(2008 November 7th, Interviewed by the Public Relations Group, Office of the President)
Research of Cartilage Regeneration by Professor Mitsuo Ochi was introduced by TBS TV "Yume no Tobira" on October 25, 2009.
Click here to see the broadcast content.
Click here to see a Blog "editor's postscript" by the program creator.
Ministry of Education, Culture, Sports, Science and Technology announced a “Note regarding the decision of The 2010 fields of science and technology’s Minister of Education, Culture, Sports, Science and Technology winners etc.” on April 5, 2010. Professor Mitsuo Ochi’s “Three-dimensional culture to promote cartilage regeneration technology” won the Science and Technology Award (Science and Technology Promotion Division) for promoting scientific technology. Managing Director and Research Development Director of Japan Tissue Engineering Co., Ken-ichiro Hata and its Research and Development Department’s Katsura Sugawara were also joint winners of this award. (2010 April 5th)
Aiming to be a Knee Specialist
Professor Ochi graduated from the Faculty of Medicine at Hiroshima University in 1977, and entered the Department of Orthopaedic Surgery led by Professor (at the time) Kenya Tsuge. Upon entering the department, he diagnosed and treated many patients who had damaged cartilage due to traffic accidents or sports and patients with torn ligaments due to sports injuries with the aim of becoming "a comprehensive knee surgeon dealing with all parts of the knee be it ligaments, cartilage, or the meniscus". Players from the Hiroshima Carp baseball team and the San Flecce soccer team rely on the professor and have come to see him. In his time as a lecturer and assistant professor, he carried out over 130 ligament surgeries a year, however, in 1995, he transferred to the Shimane University Faculty of Medicine as a professor.
The population of Shimane prefecture was sparse, and sports players with injured ligaments were few. Taking advantage of his transfer, the professor's primary research focus shifted from ligaments to cartilage research and treatment. The hyaline cartilage of the knees and elbows serve as a cushion so that the hard bones of the legs or arms don't grind against one another. The cartilage has a moderate degree of elasticity and its surface is smooth and slick, which enables it to fulfill the important role of suppoting smooth joint movements. However, the cartilage also lacks in regenerative capability, and once it has been damaged, it very rarely heals itself naturally. Thus, there was no real effective treatment for osteoarthritis of the knee (condition in which cartilage of the knee wears down and causes inflammation, which in turn causes damage to joints and pain) or for traumatic cartilage defects often seen in sports players. In Shimane prefecture, where many elderly reside, there were many patients suffering from osteoarthritis of the knee and Rheumatoid arthritis, making cartilage the perfect subject for research.
Development of the World's First Cartilage Transplant Method
For cartilage defects, the treatment method of mosaicplast using osteochondral plugs taken from non weight-bearing areas and transferring them to the defect area made it difficult to smoothly form the articular surface since the transferred plugs differed in shape from the original. Also, in cases of large defects, it was almost impossible to repair as the amount of cartilage which can be taken is limited. In 1994, Swedish doctor Lars Peterson, Ph.D., presented a method by which cartilage cells from the patient were extracted, and then cultivated outside of the body. Then, periosteum was sutured on the defect area like a patch, and the cultivated cartilage cells in a suspension liquid are then injected into the gap between the patch and the defective area. With this method, however, if the patient moved before the cells had attached themselves, it was thought that the cells would leak out from the gaps in the periosteum patch. So, the professor thought of a new method which would overcome this weak point in the Swedish method: "When we culture condrocytes in the gel 3D culture, we make cartilage-like tissue, then implant the tissue on the cartilage defect and implant a periosteum over the tissue. The tissue can relatively attach themselves without leaking." He immediately established a cell culture lab for humans at the Shimane University Faculty of Medicine and began trials of the new method.
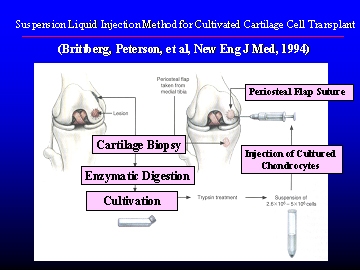
Suspension liquid injection method for cultivated cartilage cell transplant
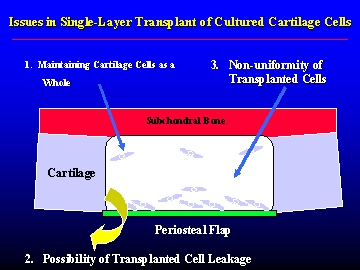
Cross-section of the transplant site (single-layer cultivation)
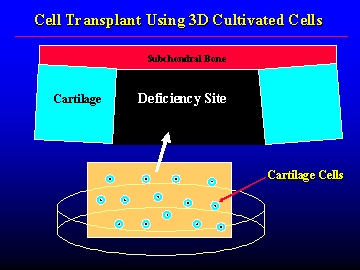
Cross-section of the transplant site (3D cultivation)
The professor spent his days looking for a material that would not only create a solid structure, but would also serve as safe "scaffold", and it wasn't long before he found his answer in "atelocollagen", a type of collagen used to treat wrinkles in dermatology and plastic surgery. The professor himself had used it in research on artificial nerves, and also knew that it had few adverse side effects.
By taking normal cartilage fragments from the non weight-bearing area of the femur, and then upon breaking it up into small pieces and treating it with enzymes to obtain isolated chondrocytes, the professor cultivated the chondrocytes inside the atelocollagen, and after 3 weeks, the cells were surrounded by an extra cellular matrix and obtained a jelly-like hardness. This is implanted into the defect site, and then covered with a cap made of periosteum, which is sewn on as to prevent leaks, from the tibia. After implantation, the atelocollagen is gradually absorbed by the body and dissolves.
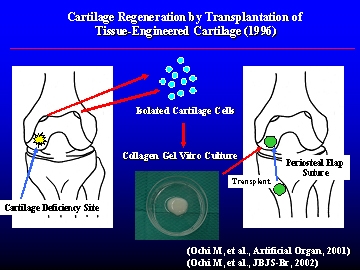
Cartilage regeneration by transplantation of a tissue-engineered cartilage
In 1996, the professor began the world's first "clinical trial to transplant three-dimensional, cultured atelocollagen autogeneous chondroytes embedded in Atelocollagen gel".
In April 2002, the professor returned to his post at HU, with his transplant method continuing to gain excellent results. In 2004, he was jointly awarded the Science Council of Japan's Presidential Award at the Cabinet Office-sponsored Industry-Academic-Government Collaboration Promotion Meeting. The Presidential Award is awarded to cases which have been recognized as especially remarkable achievements or services from the academic standpoint, and have already received the Industry-Academic-Government Collaboration Promotion Meeting's Distinguished Service Award. While shouldering the important jobs of Deputy Director and Director of the University Hospital, as well as the University's Executive of Medical Affairs, the professor, a self-claimed "clinician through-and-through", conducts surgeries in between his work in research, education, and medical practice.
To Spread Technology Far and Wide
A variety of cartilage regeneration treatments can be performed using this method, and in some cases, the repair is so complete that the repaired cartilage cannot easily be distinguished from the surrounding cartilage. At present, in order to further spread cartilage regeneration using tissue-engineering technology, technology transfer to a regenerative medicine venture business in Aichi Prefecture is taking place, and clinical trials have ended at 5 hospitals across the country (HU, Shimane University, Hokkaido University, Tokyo Medical and Dental University, etc). The company will also soon apply for manufacture and sales approval, looking toward actual implementation of the professor's method.
The Next Idea: Regenerating Cartilage and Bones Using Magnets
"Cartilage damage differs in each patient."
"With our method, we have to make incisions to the patient's knee two separate times: once to get the cartilage cells and once to implant the cultured tissue."
"This method is not suitable for all cases."
In this manner, the professor calmly states the issues that lie ahead. "I'm always thinking of a solution", says the professor, as the next idea comes into place.

"The cartilage is wearing down."
While thinking of whether it would be possible to use an endoscope (knee arthroscopy) to see where to inject the chondrocytes instead of making incisions into the patient, the professor was struck with an idea, an in September of this year, the professor and his team announced that they had developed a treatment method in which cells which have been cultivated mixed with iron powder are drawn to the defect site using a high-powered magnet (patent pending).
The team uses mesenchymal stem cells, which differentiate into bones, cartilage, or muscle (*1). Bone marrow extracted from the patient's body is cultured overnight in a medium containing fluid along with magnetic beads (circumference of 10 nanometers; nano=1 billionth of a meter) used as an imagining agent when taking MRIs(*2), and a special medicine. Then we get magnetically labeled mesenclymal stem cells.
(*1) A cell which is undifferentiated, i.e. has the potential to become various types of different cells such as muscle, bone, fat, etc, and also has the ability to self-replicate. The mesenchymal stem cells found inside of bone marrow are typical example of these cells, and as it is relatively easy to isolate them from the patient's bone marrow, it is hoped that they can be used in clinical applications for bone and cartilage regeneration.
(*2) Magnetic Resonance Imaging: machine which utilizing the resonance phenomenon which occurs between magnetic fields and the cell’s nucleus to display images of the organs inside of living beings. By using a high-powered magnetic field, images become more detailed and high-contrast. As it is possible to view soft tissues such as cartilage, doctors are able to view the condition of knee joints in detail. The exam is also makes use of magnets, which do not carry adverse effects as radiation does.
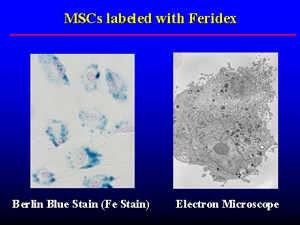
Cells containing magnetic beads
When the steam cells are injected, a high-powered magnet outside of the body is used to collect the cells to the defect site on the bone or cartilage, and within about 3 weeks, the steam cells become cartilage or bone to compensate for the defect. The amount of time that the magnetic force is used varies depending on the size of the defect; however, it generally takes about 1 to 3 hours.

Spanner attached to the magnetic force generator (at maximum magnetic force, it is possible to hold a 600g metal spanner on the electromagnetic surface).
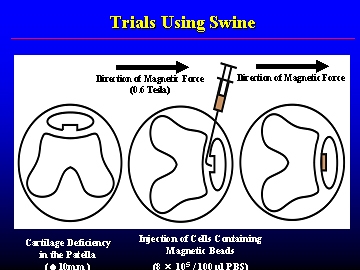
Cells attached to the chondral defect using magnetic force (image from trials using swine).
In animal experiments using pigs and in experiments using cartilage from humans, they were able to successfully regenerate cartilage at a defective site of more than 1 cm-squared, and it was also confirmed that the cells function just as the originals. The iron particles are finally used to form hemoglobin, which brings oxygen to red blood cells. As the iron particles used in the procedure are already in use in the medical field, there is little concern of adverse side effects. Although there are still many issued which must be resolved before the start of human clinical trials, with this method, there is comparatively less stress on the patient than surgery, as they method requires only an injection and a magnet. The procedure can also be repeated multiple times, and it is anticipated that it will have a great effect. This procedure is not only making headlines in Japan, but was also covered by one of the four large newspapers in Taiwan, The Liberty Times, who ran an article on the procedure on September 12.
Providing an Environment for Thought
Researchers who gather with a love of learning are not limited only to Japan. In the research lab of the Graduate School, there are graduate students from Egypt and Thailand taking courses, and there are also short-term clinical students from Malaysia. The professor's advice to young researchers is this: "Be aware of the issues, and always consider how those issues can be resolved!" The professor, and strives to give students the chance to interact with already top-class researchers or clinicians by inviting well-known researchers from inside and outside of Japan to visit and creating an environment for students to hear their lectures and discuss matters with them, which will provide them with motivation and stimulation. For three years and counting, the professor himself has given lectures abroad 27 times in America, Europe, and Asia, including giving highlight lectures at International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (Florence, Italy) and at European Society of Sports Traumatology, Knee Surgery and Arthroscopy (Innsbruck, Austria), and invited to lecture at the American Academy of Orthopaedic Surgeons. It seems that the professor's circle of new academic and research exchange is growing wider by the day. "I want young researchers in Hiroshima to aim for the world - they are sufficiently talented," says the Professor with hope.
Afterword
"Universities have the capability to create environments. But it's not as if universities can do everything alone. I believe that it's the result of the efforts of many, the harmony of the power of individuals which becomes the complete power of the university. That goes for research and for community cooperation as well," says the professor, but there is a lack in enthusiasm and vigor. Professor Ochi, who has continued to follow the motto "Always be thinking," and turned his thoughts into realities, it is performing high-aiming, top-level research and teaching the knowledge gained to the next generation which is important. Providing equal and high quality medical treatment to patients based in results gained from research isn't something exceptional - it should be expected. When I interviewed the professor and excitedly asked when clinical trials would begin, Professor Ochi gave an eloquent response: "Would you want to give your family a medical treatment still in its incomplete stage? I will not give patients a treatment that I wouldn't give my own family. There are still miles to go before we can begin the process of clinical testing." This interview made me think about the importance of patient and steady progress forward every day. (O)

 Home
Home