By Hiroshima University Department of Public Relations
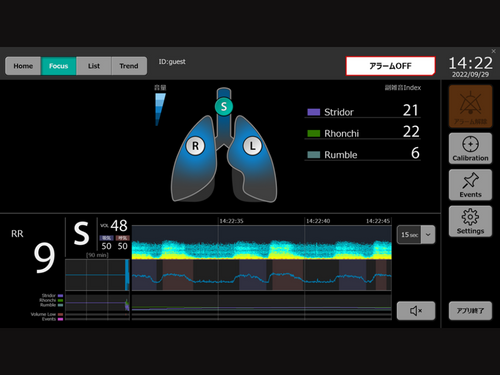
The interface of the continuous respiratory sound monitoring device. (Photo courtesy of Professor Nobuaki Shime)
Researchers developed a novel device that detects abnormal breathing sounds to predict whether an ICU patient is likely to suffer from respiratory complications after removal from a mechanical ventilator, alerting intensive care teams to the need for emergency interventions at an early phase after extubation.
The monitoring device designed by Hiroshima University (HU) emergency and critical care medicine specialists is powered by an AI they previously created and trained to analyze and visualize abnormal respiratory sounds. The device’s creation was funded by the Japan Agency for Medical Research and Development (AMED).
In their pilot study published in the Journal of Clinical Monitoring and Computing, the researchers detailed how converting abnormal respiratory sounds into quantitative values as a real-time monitor through their device proved to be useful in predicting respiratory complications after extubation. It could help healthcare professionals in predicting respiratory failure and other life-threatening airway emergencies.
According to the researchers, respiratory failure occurs in 10-20% of post-extubation cases in ICUs, with a mortality rate of 25-50%. Non-invasive ventilation (NIV), such as oxygen delivery via face mask, or high-flow nasal cannula (HFNC) may prevent respiratory failure and the need for reintubation. However, they noted that the high cost of these devices makes it difficult to provide them to all patients who are removed from breathing support.
Predicting the likelihood of respiratory failure and other breathing difficulties is useful in determining whether a patient will need an unscheduled NIV or HFNC, reintubation, or a more invasive procedure such as cricothyroidotomy, which involves puncturing the throat to create an airway.
“Respiratory failure in the intensive care unit (ICU) frequently occurs, particularly in patients after extubation, but there has been a lack of sufficient monitors to detect such abnormalities earlier,” said Nobuaki Shime, professor at HU’s Graduate School of Biomedical and Health Sciences, who led the research team.
Shime noted that auscultation of the respiratory system, or listening to breathing sounds with a stethoscope, could be a “simple and useful method to assess respiratory status.” It is, however, “subjective and non-continuous.”
Their device solves these problems by providing a continuous monitoring system for respiratory sounds as well as improving prognosis by assisting critical care staff in objectively evaluating respiratory status.
Respiratory sound, including stridor, rhonchi, gargling, wheezes, and crackles, are captured at multiple locations by a sensor and visualized in real-time as a spectrogram. Their machine learning algorithm then analyzes and quantifies these frequency signals. The algorithm calculated the quantitative value (QV) of gargling, stridor, and rhonchi in the cervical region or neck and wheezes, rhonchi, coarse crackles, and fine crackles in the thorax area or chest.
The continuous respiratory sound monitoring device in action. (Photo courtesy of Professor Nobuaki Shime)
The study included 57 patients. Eighteen patients experienced the composite outcome, requiring airway and respiration medical interventions within 48 hours after extubation. The rest belonged to the non-outcome group.
According to the researchers, the QVs of stridor and rhonchi in the cervical region were significantly higher in the composite outcome group than in the non-outcome group. Meanwhile, the QVs of wheezes, rhonchi, and coarse crackles in the anterior thorax region were significantly higher in the outcome group than in the non-outcome group.
The QV of fine crackles in the bilateral lateral thorax region was significantly higher in the outcome group than in the non-outcome group. They also stated that inhalation sound volume (average of 5 breaths) in the cervical region immediately after extubation was significantly louder in the outcome group (63.3 dB) than in the non-outcome group (54.3 dB).
Although the device’s predictive score remains to be validated due to the small sample size, the researchers believe that the continuous objective evaluation of respiratory sounds made possible by their apparatus might lead to increased patient safety in ICUs after extubation.
“It will definitely contribute to improving the quality of the cardiorespiratory monitoring system to detect respiratory abnormalities earlier,” Shime said.
Their research received the 2022 Best Presentation Award from the Japanese Airway Management Society.
(Research news authored by Mikas Matsuzawa)

 Home
Home